A diabetic foot ulcer is one of the most common complications of uncontrolled diabetes. It occurs when an open sore or wound does not heal properly and gets ulcerated. This ulcer usually occurs at the bottom of the foot.
It is estimated that nearly 15-20 percent of diabetic people develop foot ulcers at some point in life. The risk of developing diabetic foot ulcers increases with the duration of diabetes. Thus, it is most common in people having diabetes for more than 10 years. It also affects older people more than younger ones.
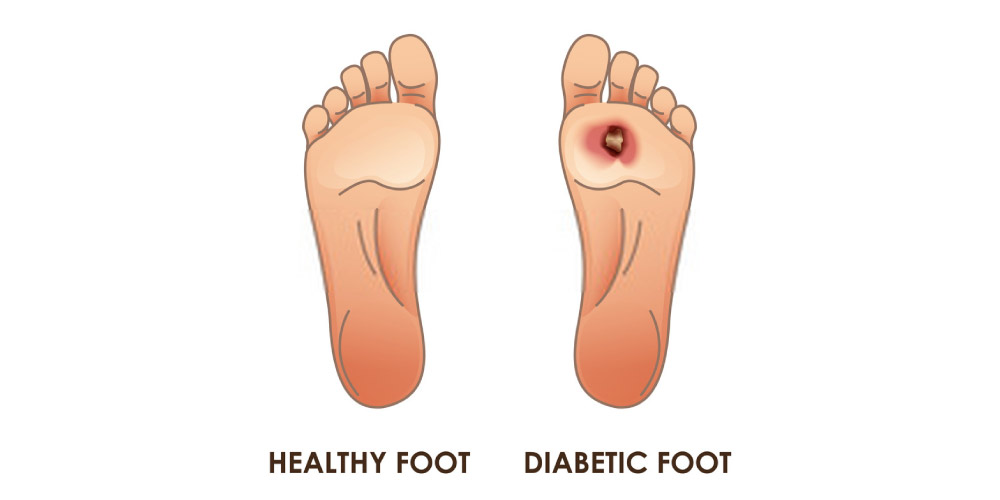
Table of Contents
What are the symptoms of Diabetic Foot Ulcers?
Diabetic foot ulcers usually start with a small injury or trauma to the foot. It can be a scratch or cut that can cause an ulcer to form. These are some signs and symptoms that may indicate the development of diabetic foot ulcers:
- Swelling and irritation around the wound
- Foul-smelling discharge or leakage from the wound
- Formation of a black tissue around the wound
- Numbness in the area
- Thickening of the skin surrounding the ulcer
- Experiencing pain when you touch the wound
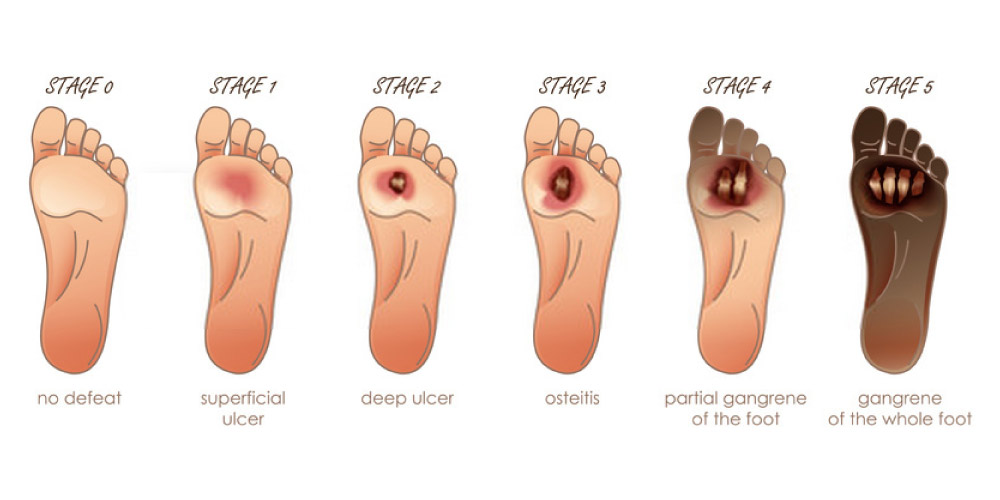
Based on the severity of the condition, there can be 6 stages in the development of a diabetic foot ulcer.
0: Intact skin
1: Superficial Ulcer
2: Deep ulcer extending to the tendon, bone or joint
3: Deep ulcer along with the formation of an abscess
4: Gangrene(death of tissues) in the forefoot
5: Gangrene affecting the complete foot
If you notice any of these symptoms, consult a doctor immediately. Diabetic foot ulcers have a tendency to worsen over time and if left untreated, they can lead to serious complications and infections. Diabetic foot ulcers may even lead to foot amputations in serious cases.
What are the causes of Diabetic foot ulcers?
Even minor cuts, injuries, small blisters, or wounds can initiate diabetic foot ulcers. This happens because the presence of diabetes slows down the healing process. Along with this, most diabetes patients become ischemic over time which means they lose sensations in the nerves due to which they don’t feel pain. As a result, the wound or cut becomes more serious and becomes prone to ulcers and infections without the knowledge of the patient.
The following are the reasons due to which the healing process slows down in diabetes:
Uncontrolled blood sugar leads to impaired healing
Due to an increased level of glucose in the blood, the cell walls become stiff and rigid. This affects the flow of blood through the blood vessels and therefore not enough red blood cells can reach the wounded tissue, leading to slower healing.
Peripheral Neuropathy caused due to diabetes
Prolonged diabetes and high blood sugar levels tend to damage the sensory, motor, and autonomic nerves. When the sensory nerves in an area are damaged, the area becomes numb and the person is unable to feel pain, temperature, or other sensations in that area. Due to this, in many cases, you may not even be aware of minor injuries or trauma to your feet and would not receive proper treatment in time. This wound or cut may get infected over time and transform into a diabetic foot ulcer.
Diabetes causes Peripheral Artery Disease
Due to diabetes, blood vessels become inflamed and hardened. It also leads to the narrowing of the arteries due to which the flow of oxygen, glucose, and essential nutrients to the wounded tissues are obstructed. Due to lack of oxygen, the wound becomes more prone to infections, and ulcers can easily develop.
What are the risk factors for Diabetic Foot Ulcers?
In addition to the aforementioned causes, there are also certain factors that increase the chances of developing diabetic foot ulcers. Some of the risk factors for diabetic foot ulcers include:
- Being overweight
- Not maintaining proper hygiene
- Wearing poorly fitted shoes
- Regular consumption of alcohol
- Kidney, heart, or eye disease associated with diabetes
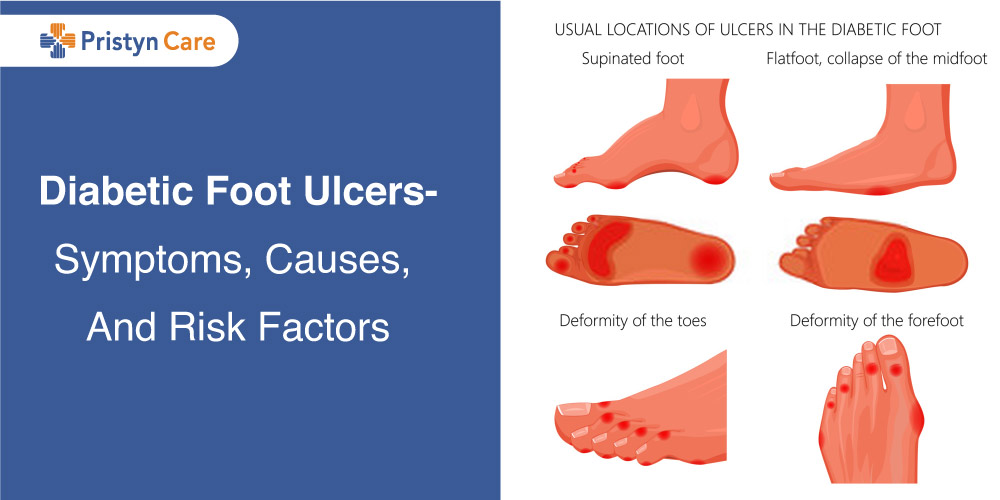
- Deformities in the foot
- A history of ulcers in the feet
- Being a smoker
If you relate to any of these risk factors, you should be extra cautious with your blood sugar levels. Try to avoid injuries to the feet as much as possible.
You should be careful at all times and consult a doctor for the slightest of injuries or wounds.
If you notice any of the symptoms of foot ulcers, consult a doctor immediately. Diabetic foot ulcers have a tendency to worsen over time and if left untreated, they can lead to serious complications and infections. Diabetic foot ulcers may even lead to foot amputations in serious cases.
Now that you understand how severe this condition can be, you must be wondering how diabetic foot ulcers can be treated.
Let’s get an insight into the treatment procedures for diabetic foot ulcers.
What are the treatment procedures for diabetic foot ulcers?
In the initial stages of foot ulcers, debridement may prove to be an effective solution. In debridement, your doctor uses a scalpel to remove the dead and infected tissues from the ulcerated wound. The doctors cover the wound with a sterile bandage and replace it regularly. Besides debridement, other non-surgical treatment methods for diabetic foot ulcers include off-loading or Total Contact Casting and hyperbaric oxygen therapy.
(Also read: How to get rid of diabetic foot ulcer?)
Along with debridement, your doctor may also enforce infection control methods. Your doctor may prescribe antibiotics that help to prevent infection in the wound. Usually, ointments and creams help in fastening the healing process.
In serious cases, however, surgery may be required. If the underlying cause of the ulcer is a vascular problem, vascular surgeries like atherectomy, balloon angioplasty, foot & ankle surgery, and vascular reconstruction are the treatment options depending on the severity of the condition. In many cases, surgical and non-surgical procedures are combined to effectively treat diabetic foot ulcers.
Fortunately, these vascular surgeries are available at Pristyn Care. Our team of experienced surgeons is capable enough to perform these procedures efficiently. If you have any queries about vascular surgeries, you can call us. Our medical coordinators will book the appointment with the best vascular surgeons for you.
Also Read:
- Diabetic foot ulcer home treatment
- Home remedies for mouth ulcers?
- What are stomach ulcers? How poisonous can they be for your health?















