
Select City
Bariatric surgery, commonly known as weight-loss surgery, offers a powerful solution for individuals who have struggled to lose weight through diet, exercise, or medications. It is more than a cosmetic procedure; it is a life-changing treatment that can significantly reduce the risk of diseases such as type 2 diabetes, heart disease, hypertension, sleep apnea, and even some cancers.
Bariatric surgery, commonly known as weight-loss surgery, offers a powerful solution for individuals ... Read More




Free Cab Facility

No-Cost EMI

Support in Insurance Claim

1-day Hospitalization

USFDA-Approved Procedure
Choose Your City
It help us to find the best doctors near you.
Ahmedabad
Bangalore
Chennai
Delhi
Hyderabad
Kochi
Pune
Delhi
Hyderabad
Pune
Mumbai
Bangalore
Bariatric surgery refers to a weight loss treatment that includes a group of surgical procedures designed to help people lose weight by making changes to their digestive system. These procedures either reduce the size of the stomach or change how the body absorbs food.
It is typically considered for individuals who:
Bariatric surgery is not a quick fix. It requires long-term lifestyle changes, including a strict diet, exercise, and regular medical follow-ups.

Fill details to get actual cost


Bariatric surgery is not a one-size-fits-all weight loss treatment. Different people may benefit from different procedures depending on their health condition, body mass index (BMI), and lifestyle. Each type of surgery changes the way the digestive system handles food, either by limiting how much a person can eat, how nutrients are absorbed, or both. This section explores the most commonly performed gastric surgery types; what they are, how they work, and why someone might choose one over another.
Gastric Bypass Surgery is one of the most established and widely performed bariatric procedures around the world. It works by creating a small pouch from the stomach and connecting it directly to the small intestine. In this gastric bypass surgery, a large portion of the stomach and part of the intestine are removed, leading to reduced calorie absorption and a feeling of fullness after eating a small amount.
Key Features and Benefits of Gastric Bypass Surgery:
Sleeve Gastrectomy is one of the gastric surgery types that involves removing about three-quarters of the stomach. What’s left behind is a narrow, sleeve-like structure. This procedure does not divert intestines like gastric bypass. It decreases levels of hunger-stimulating hormones such as ghrelin and assists in restricting food consumption.
Key features and benefits:
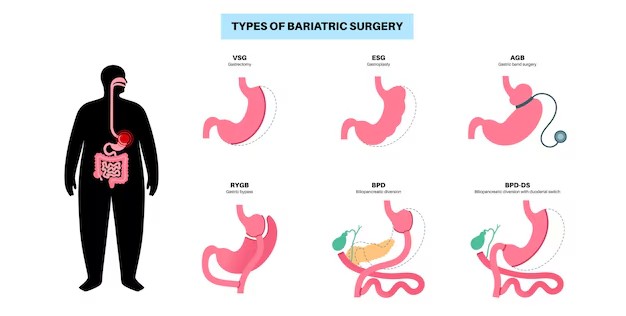
In this procedure, a silicone band is placed around the upper part of the stomach. It creates a small pouch that limits how much food a person can eat at once. The tightness of the band can be adjusted over time by injecting or removing saline through a port placed under the skin.
Key Features and Benefits of Adjustable Gastric Banding:
This is a more complex gastric bypass surgery that combines two major steps: first, a sleeve gastrectomy is performed; then the small intestine is divided and rerouted. This drastically reduces calorie and nutrient absorption. BPD/DS is often reserved for patients with severe obesity or those who have not succeeded with other surgeries.
Key Features and Benefits of Biliopancreatic Diversion with Duodenal Switch:
Each of these surgeries has its own role depending on patient health, weight goals, and medical conditions. Choosing the right one involves careful consultation with a bariatric surgeon and a detailed understanding of the risks and benefits.
When considering gastric bypass surgery, it’s important to understand that not all procedures are the same. Each type of surgery offers a different level of weight loss, recovery time, and risk. While all aim to help patients lose excess weight and manage related health issues, they work in slightly different ways. The gastric surgery types comparison will give a clearer view of how procedures like Gastric Bypass, Sleeve Gastrectomy, Adjustable Gastric Band, and BPD/DS differ in effectiveness, safety, and long-term results.
Here’s a quick comparison of the most common types of gastric surgery types:
| Surgery Type | Weight Loss (after 1 year) | Hospital Stay | Risk Level | Reversible |
| Gastric Bypass | 70% of excess weight | 2–3 days | Moderate | No |
| Sleeve Gastrectomy | 60% of excess weight | 1–2 days | Low | No |
| Adjustable Gastric Band | 40% of excess weight | 1 day | Low | Yes |
| BPD/DS | 70–90% of excess weight | 3–4 days | High | No |
Preparing for bariatric surgery is a vital part of the weight loss journey. It sets the stage for a smoother surgery, reduces complications, and improves long-term outcomes. This stage can begin weeks or even months before the actual procedure, depending on one’s health condition and the type of surgery planned. Here is a detailed look at what’s involved in getting ready for the weight loss surgery:
One has to undergo a thorough health check to confirm that they are fit for gastric bypass surgery. This usually includes:
Any existing conditions, such as type 2 diabetes, high blood pressure, PCOS, or obstructive sleep apnoea, need to be brought under control before surgery. In some cases, a specialist team (e.g., endocrinologist, cardiologist, pulmonologist) may be involved.
Working with a registered dietitian is essential. A personalised bariatric meal plan is provided that helps to:
Newer protocols also involve body composition analysis (via DEXA scans or bioimpedance) to track lean mass and fat loss more accurately before and after surgery.
Mental readiness is as important as physical preparation. The patient may be referred to a clinical psychologist for:
This step helps lower the chances of post-operative regret, food addiction relapse, or unrealistic expectations.
Certain habits must be addressed before undergoing bariatric surgery:
Newer tools like wearable activity trackers and app-based nutrition logs are now widely used by bariatric teams to guide the progress.
A few weeks before surgery, the surgeon provides detailed instructions that include:
Some hospitals also use Enhanced Recovery After Surgery (ERAS) protocols. These include carb-loading drinks before surgery, minimal fasting periods, and early mobilisation after surgery to reduce hospital stay and boost healing.

Diet & Lifestyle Consultation

Post-Surgery Recovery Follow up

Free Cab Facility

24*7 Patient Support
Recovery and post-operative care are crucial parts of the weight loss journey after bariatric surgery. Once the surgery is complete, the body and lifestyle will undergo major changes. Proper care during this phase helps avoid complications and ensures long-term success.
After surgery, patients typically stay in the hospital for 1–4 days, depending on the type of surgery. During this time:
One of the most important parts of post-operative care is the bariatric diet plan, which typically progresses in four phases:
After around 2 months, most patients can begin eating regular solid foods in small, frequent portions.
Because bariatric surgery reduces food intake and/or nutrient absorption, lifelong supplements are essential. Commonly prescribed supplements after the various gastric surgery types include:
Regular blood tests are required to check levels and prevent deficiencies.
Patients are encouraged to start light walking soon after surgery. Over time, exercise becomes a key part of long-term success. A typical plan includes:
Bariatric surgery brings emotional and psychological changes. It is normal to feel overwhelmed, especially when adapting to new eating habits and body image. That’s why:
After surgery, regular follow-up visits are essential to check healing, nutrition, and progress. These include:
If any issues arise, like nausea, vomiting, hernia, gallstones, or rapid weight regain, the bariatric team provides medical or surgical solutions.
Even with careful post-operative care, some complications may occur. These include:
Recognising symptoms early and staying in touch with the healthcare team can prevent most of these complications from becoming serious.
Bariatric surgery is a powerful tool for weight loss and health improvement, but like any major procedure, it comes with certain risks and potential complications. Understanding these issues in advance helps patients make informed choices and prepare for better recovery.
These complications occur soon after the operation and are typically linked to the surgical procedure itself or the recovery period. While most patients recover without problems, these issues may arise:
Internal bleeding may occur at the surgical site, especially in the first 24–48 hours. Symptoms include dizziness, low blood pressure, and visible blood in drains or vomit.
Infections at incision sites or inside the abdomen (abscesses) are possible. Signs include redness, fever, pus discharge, and pain at the site.
The risk of DVT is higher after major surgeries. If a blood clot travels to the lungs (pulmonary embolism), it can be life-threatening. Early movement, compression stockings, and medications are used to reduce this risk.
This happens when a connection made between the stomach and intestine leaks digestive juices. Though rare (0.5–2% of cases), it is serious and may require immediate surgery.
Due to the reduced stomach size, overeating or poor food choices can cause vomiting, especially in the early post-op weeks.
This is common after gastric bypass. It occurs when sugary or high-fat food moves too quickly into the small intestine, causing nausea, cramps, diarrhoea, and dizziness.
While bariatric surgery has many long-term benefits, certain complications may develop over time. These are often linked to nutrient absorption, lifestyle habits, or anatomical changes.
Due to reduced food intake and absorption, the body may lack essential nutrients like:
| Nutrient Deficiency | Common Symptoms |
| Iron | Fatigue, pale skin, weakness |
| Vitamin B12 | Numbness, memory problems |
| Calcium & Vitamin D | Bone pain, brittle bones |
| Folate | Anaemia, mood issues |
| Protein | Hair loss, muscle wasting |
Lifelong vitamin and mineral supplements are required to prevent these issues.
Rapid weight loss can lead to gallstone formation, which may cause pain, nausea, or even require gallbladder removal surgery.
Internal or incisional hernias (bulges of organs or tissue) may appear at surgical sites and might need repair.
Narrowing of the digestive tract can happen after surgeries like gastric bypass or sleeve gastrectomy. It can make eating difficult and may require a procedure to stretch or correct the narrowing.
While surgery reduces stomach size or food , it doesn’t stop old eating habits. Emotional eating, lack of exercise, or poor food choices may lead to partial weight regain, especially 2–5 years after surgery.
Some patients experience:
Mental health support, counselling, and therapy are strongly recommended.
Women are usually advised to wait 12–18 months after surgery before becoming pregnant. This ensures weight stabilisation and avoids risks to the mother and baby from malnutrition.
After certain surgeries like Roux-en-Y Gastric Bypass, alcohol is absorbed faster and more strongly. Patients are usually advised to avoid or limit alcohol post-surgery.
| Complication | Approximate Risk |
| Death (within 30 days) | Less than 0.3% |
| Major complications (short-term) | 17% |
| Anastomotic leak | 0.8–1.5% |
| Nutritional deficiencies | Up to 35% without supplements |
| Gallstones after rapid weight loss | 10.4–52.8% |
| Weight regain (partially) | 20–30% within 5 years |
Weight loss is only one of the many health benefits of bariatric surgery. Numerous studies have shown that patients undergoing these procedures can experience:
In fact, one long-term study published in the New England Journal of Medicine found that patients who underwent bariatric surgery had a 40% lower risk of death over ten years compared to those who did not.
The bariatric surgery cost can vary based on the city, hospital, and type of procedure.
| Type of Surgery | Approximate Cost (INR) |
| Gastric Bypass | ₹3,00,000 – ₹5,00,000 |
| Sleeve Gastrectomy | ₹2,50,000 – ₹4,50,000 |
| Adjustable Gastric Band | ₹2,00,000 – ₹3,50,000 |
| BPD/DS | ₹4,00,000 – ₹6,00,000 |
Some insurance companies in India now cover bariatric surgery if deemed medically necessary. Patients should consult their insurer and healthcare provider for eligibility.
While bariatric surgery is a highly effective treatment for obesity and related health conditions, it is not appropriate for all individuals. The procedure is generally not recommended for those who:
For individuals who fall into these categories, non-surgical weight management approaches such as medically supervised weight loss programs, behavioural therapy, or pharmacological treatments may offer safer and more suitable alternatives.
Bariatric surgery is a medically recognised treatment for individuals with severe obesity and related health complications. Although it is not a cure-all, it has demonstrated effectiveness in improving physical health, enhancing quality of life, and supporting sustained weight loss when combined with appropriate follow-up care.
For individuals who have not achieved adequate results through conventional weight loss methods, consulting a qualified bariatric surgeon can help determine whether bariatric surgery is a clinically appropriate option. Consult a Pristyn Care specialist to assist you in understanding your treatment choices.
Jasleen began her journey with Pristyn Care feeling anxious but hopeful. Her consultant, Khushi, guided her every step managing insurance, appointments, and all formalities so she could focus on recovery stress-free.
Under the care of Pristyn Care, Jasleen underwent surgery with confidence. His reassuring nature and expertise made the experience smooth and comforting. Post-surgery, the dietitian, supported her with regular diet guidance and motivation.
From 135 kg to 88 kg, Jasleen’s transformation is a story of determination and care. She continues her journey, grateful for the constant support and compassion shown by the entire Pristyn Care team.

Procedures like gastric bypass and sleeve gastrectomy are permanent. Gastric banding is reversible, though reversals are uncommon and typically done only for medical reasons.
Temporary hair loss may occur within 6 to 9 months after surgery due to rapid weight changes and nutritional shifts. It is usually reversible with adequate nutrition and supplements.
Recent innovations in bariatric surgery include non-invasive options like endoscopic sleeve gastroplasty and precision-based robotic-assisted procedures. Enhanced Recovery After Surgery (ERAS) protocols and AI-driven tools are also improving outcomes and reducing recovery time.
Travelling is generally safe after the initial recovery period, but long-distance travel should be avoided in the first few weeks. Carry medical records and follow dietary guidance while travelling.
Some patients opt for body contouring surgery after significant weight loss to address excess skin. This is a decision on an individual basis and not on a medical need.
Most people resume light work 2 to 4 weeks post-surgery, varying with the type of procedure and healing rate. Always follow the surgeon’s advice.
Yes, but any subsequent surgery will need to take into account variations in anatomy and nutritional status. Always tell your healthcare team about your history of bariatric surgery at the time of preoperative planning.
The decision regarding the most appropriate bariatric procedure depends on a variety of factors such as body mass index (BMI), pre-existing medical conditions, lifestyle factors, and desired weight loss. A thorough medical assessment determines the best surgical option.
Yes, in particular instances, revision surgery can be needed because of complications or inadequate weight loss. Whether a second procedure is necessary is based on individual clinical judgment and surgical experience.
Hunger usually decreases after surgery, especially with procedures that reduce hunger hormones like sleeve gastrectomy or gastric bypass.
 Medically Reviewed By:
Medically Reviewed By:
Shivaji Gurav, 50 Yrs
Recommends
Its been a year since my bariatric surgery done by dr. shashank shah in pune. I cant even explain how much reliefed i am right now after loosing weight. at 90 kg at the moment. dropped from 120kg last year
Pamdari Narendar, 32 Yrs
Recommends
it was very good treatment procedure from the start to the end. Staff of Dr shashank shah is very helpful. Really belived that this obesity will take my life. but after treatment it looks a hope for my pain.
Subrat, 52 Yrs
Recommends
I had done my obesity treatment. Its was good.
Vandana Sharma, 25 Yrs
Recommends
I was very fat due to some hormones or what so ever reason. i cannot explain the pain i had in my legs due to overweight body. Thanks to dr. shashank shah. After surgery i am feeling more confident and light weight. my urge to over eat food has also resolved in it.
Mihil Sharma, 25 Yrs
Recommends
My over weight surgery went really good and smooth. Didnt have any issue aftewr surgery. Dr shashank was exceptional in explaining so complicated things in such layman terms.
Tajinder Arora, 36 Yrs
Recommends
My weight loss treatment started a 1.5 month ago with all the diets and medications. I can't believe on seeing the results. Highly recommended yaar.
.svg)
.svg)