
Select City
Get safe and advanced treatment for unappealing spider veins. At Pristyn Care, we leverage minimally invasive laser technology and sclerotherapy to treat spider veins or telangiectasia to provide effective results and improve the appearance of bluish, purple veins. Book an appointment with the best vascular surgeons in India and plan the treatment.
Get safe and advanced treatment for unappealing spider veins. At Pristyn Care, we ... Read More




Free Cab Facility

No-Cost EMI

Support in Insurance Claim

1-day Hospitalization

USFDA-Approved Procedure
Choose Your City
It help us to find the best doctors near you.
Bangalore
Coimbatore
Delhi
Hyderabad
Kochi
Mumbai
Patna
Pune
Vijayawada
Delhi
Hyderabad
Pune
Mumbai
Bangalore
Spider veins are small, visible blood vessels that appear just under the skin, mostly on the legs and face. While they are usually harmless, they can cause discomfort such as aching, itching, or burning in some people. In India, the number of people seeking treatment for spider veins is rising, as both cosmetic and medical concerns grow. According to a report by the Indian Journal of Dermatology, around 20-30% of the adult population may develop spider veins, with women being more frequently affected.
Modern treatment options are offering visible improvements, especially when skilled specialists perform it. From minimally invasive procedures to laser-based methods, these treatments are helping individuals regain confidence and physical comfort. The results are often measurable through clear before and after changes, both in appearance and symptoms. The upcoming sections explore popular techniques, recovery timelines, expected results, and safety standards associated with such treatments in India.

Fill details to get actual cost
Spider veins often appear in thin, web-like shapes, usually red, purple, or blue in color. These lines commonly show up on the thighs, calves, and ankles. They form when tiny blood vessels widen or stretch due to pressure. Unlike varicose veins, spider veins stay close to the skin’s surface and are smaller in size.
Several factors can trigger their appearance. Long hours of standing, hormonal changes, weight changes, age, and genetics all play a role. In some cases, mild itching or a warm sensation may occur. Although they rarely pose health risks, many people feel self-conscious or uncomfortable. Various treatments are now available to improve the appearance of affected areas and support healthier vein function.
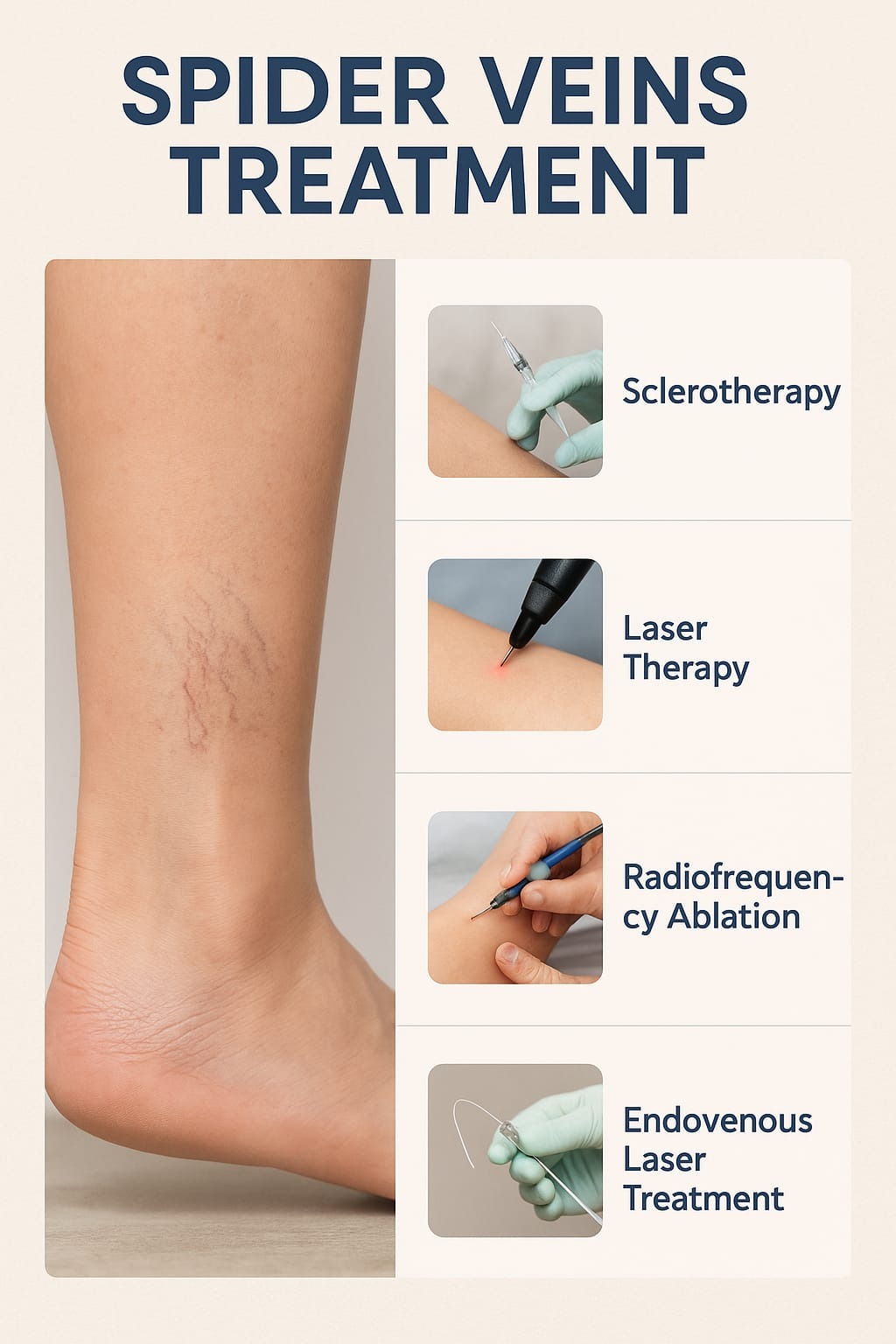
Several safe and effective methods are available today to treat spider veins. These treatments help reduce or completely remove the visible veins, offering both medical and cosmetic benefits. The choice of treatment depends on the severity of the veins, skin type, and the patient’s health condition.
Sclerotherapy
This is one of the most common techniques. Doctor injects a solution into the affected vein, causing it to collapse and eventually fade away. It’s a quick outpatient procedure with minimal downtime. Spider Veins Treatment before and after photos often show a clear improvement within a few weeks.
Effectiveness rates range from 90–95%, especially when followed by wearing compression stockings for at least two weeks.
Laser Therapy
This needleless method uses focused laser light to heat and destroy spider veins. It’s especially useful for smaller veins and for areas like the face. Results are gradual, but effective. One study from JAMA Dermatology found that sclerotherapy achieved better cosmetic results for leg spider veins, while laser worked better for small facial veins.
Intense Pulsed Light (IPL)
IPL uses a broad range of light wavelengths to treat spider veins. It’s non-invasive but less targeted than laser, often requiring several sessions. Common side effects include redness and swelling; results are gradual and may not be permanent without maintenance.
Radiofrequency Ablation
In this technique, radio waves are used to heat the vein wall, which seals it shut. It’s more suitable for slightly larger veins and offers lasting results with minimal discomfort.
Cryo‑Laser + Cryo‑Sclerotherapy (CLaCS) – India-specific advance
CLaCS combines laser pulses with very cold sclerosant injections under vein‑viewer guidance. A case series in India treated 30 patients with isolated C1 spider veins. After two sessions, 90% had partial to complete resolution. No analgesics were needed, and there were low pigmentation rates.
Endovenous Laser Therapy (EVLT)
Although EVLT is primarily designed for larger varicose veins, it is sometimes used in combination with sclerotherapy for deeper or clustered spider veins linked to venous insufficiency. During the procedure, a fine laser fiber is guided into the vein and delivers heat to collapse it. Most patients resume normal activity within 1–2 days.
Many clinics now offer Spider Veins Treatment before and after galleries to help patients understand the expected results. Most patients see smoother skin, reduced irritation, and improved self-esteem after the treatment.
Spider vein treatment is a common choice for those looking to reduce visible veins or ease minor discomfort. Even when the condition doesn’t cause pain, it can still affect how someone feels about their appearance or day-to-day comfort. Several factors often lead people to consider treatment, especially when lifestyle, genetics, or age play a role.
People who may benefit from treatment include:
Treatment may not be right for everyone:
A proper evaluation helps decide if treatment is safe and likely to work well.
Diet & Lifestyle Consultation
Post-Surgery Follow-Up
Free Cab Facility

24*7 Patient Support
Spider veins develop when small blood vessels near the skin’s surface become weakened or damaged. The valves inside these veins, which usually help push blood in one direction, may stop working properly. This leads to a backflow of blood, causing the vessels to stretch and become more visible. Several risk factors can contribute to their development, including genetic predisposition, hormone changes, ageing, obesity, and occupations that involve long hours of standing. Past injuries, sun exposure, or conditions that increase pressure in the veins, such as pregnancy, may also play a role.
Here are the main root causes and risk factors for spider veins:
When vein valves weaken or malfunction, blood can backflow and pool in small superficial veins. This increased pressure causes the vessels to dilate and become visible just under the skin
There is a strong hereditary link. Up to 90% of people who develop spider veins have a family history of vein issues.
Hormonal changes during pregnancy, puberty, menopause, or from using birth control pills or hormone therapy can weaken vein walls and valves, increasing risk.
Extended periods of immobility impede blood flow toward the heart. The increased pressure in leg veins can lead to the development of spider veins.
As one ages, vein walls lose elasticity and valves weaken. Calf muscle strength and skin thickness also diminish, making surface veins more visible.
Being overweight increases the strain on leg veins and promotes venous dysfunction, contributing to spider vein formation.
Pregnancy increases blood volume and abdominal pressure, and hormonal shifts relax vein walls. This often leads to the appearance of spider veins, especially on the legs.
Surgical trauma, direct injury, or inflammation of the skin or veins can lead to visible spider veins in the affected area.
UV radiation can damage small facial vessels, leading to spider vessels, especially on the cheeks or nose.
Not everyone is a good candidate for spider vein treatment. Certain health conditions can increase the risk of complications. A proper medical check is necessary to ensure the procedure is safe.
A full evaluation helps avoid complications and ensures the chosen treatment fits the patient’s health profile.
Spider vein treatment doesn’t classify as a medical necessity, as the condition is often harmless and mainly cosmetic. Many individuals choose treatment to reduce the appearance of red, blue, or purple veins on the legs or face.
In some cases, when spider veins lead to symptoms such as aching, burning, or discomfort, or if they are associated with underlying venous insufficiency, medical intervention may be appropriate. A clinical evaluation determines whether treatment is required for medical reasons in addition to cosmetic concerns.
In some cases, spider veins visible on the skin may signal deeper problems such as venous valve dysfunction or blood flow reflux. If these underlying issues are not diagnosed and treated first, surface-level treatments may not be fully effective. This can lead to the return of spider veins or the appearance of new, finer veins near the treated area.
This effect is known as spider vein matting, where very thin, reddish veins form in clusters, creating a pink or red blush under the skin. It often appears after procedures like sclerotherapy or laser therapy, especially when deeper vein issues go unchecked.
To avoid such outcomes, a venous duplex ultrasound is usually recommended before treatment. This noninvasive scan checks the function of both deep and surface veins, detects valve problems or blockages, and helps plan a treatment approach that addresses the root cause, not just the surface symptoms.
A clear breakdown outlines what to expect during the sclerotherapy process. Treatment is typically done in a clinic setting and requires minimal downtime. Each step is performed carefully to ensure effectiveness and comfort.
Initial Consultation and Planning
A vein specialist conducts a physical evaluation and may use ultrasound imaging to ensure deeper veins are not affected. Medical history is reviewed, and medications that could increase bleeding are identified. This sets the stage for a safe treatment plan.
Procedure Day and Follow‑Up
Recovery and Results
This method remains one of the most preferred options for both cosmetic and functional relief from spider veins.
After spider vein treatment, visible improvement and relief from mild symptoms are commonly reported. Outcomes depend on factors such as the treatment method, vein size, and the individual’s overall vein health. The following table gives a general post spider vein recovery timeline:
| Stage | Expectation |
| Day 0–2 | Mild discomfort – compression stockings and light activity encouraged |
| Week 1–2 | Bruising/redness fade; mild itching or pigmentation possible |
| Weeks 3–6 | Noticeable fading of smaller veins; visible improvement begins |
| 3–6 months | Larger veins continue to fade; cosmetic results become clearer |
| Over months/years | New veins may develop; touch-up sessions may be required periodically |
These recovery timelines differs depending on unique factors associated with respective individuals. About 50–70% of treated veins are likely to disappear permanently after sclerotherapy; up to 80% success is typical when multiple sessions are completed.
Once veins are gone, they usually do not return in the same spot, but new veins may develop over time.
Spider veins are tiny superficial vessels that are harmless and primarily a cosmetic concern, while varicose veins are larger, deeper, and often symptomatic with potential health complications. Both share similar risk factors and benefit from preventive lifestyle measures, but varicose veins may require medical or procedural intervention.
| Feature | Spider Veins | Varicose Veins |
| Appearance | Thin, red/blue/purple lines (web-like) | Bulging, twisted, enlarged veins (blue/dark purple) |
| Size | Small (less than 1mm) | Larger (more than 3mm) |
| Location | Face, thighs, ankles | Legs (especially calves and thighs) |
| Symptoms | Often painless; may cause mild itching or burning | Aching, heaviness, throbbing, or discomfort |
| Cause | Capillary dilation, hormonal factors | Valve failure in deeper veins |
| Risk Factors | Genetics, sun exposure, hormones | Prolonged standing, obesity, pregnancy |
| Treatment | Sclerotherapy, laser treatment | EVLT, vein stripping, compression stockings |
| Health Concern | Mostly cosmetic | May lead to serious vein disorders |
Spider veins are sometimes considered a milder form of superficial venous disease; varicose veins represent more advanced vein valve dysfunction.
Treatment decisions often depend on whether veins are just cosmetic or also symptomatic/medical in nature.
Different Spider Vein treatment procedures cost differently. Here’s a list of a general range:
Regional variation:
In India, expect ₹15k–₹40k per session, with a full course costing up to ₹95,000, depending on the number of sessions and technique.
Spider veins are usually harmless but may cause discomfort or affect appearance. Treatments like sclerotherapy and laser therapy are effective and widely available. With proper care, recovery is quick and uncomplicated. Seeking early medical advice ensures better and longer-lasting results. Schedule a consultation with a trusted expert at Pristyn Care to learn more.
Reach out to Pristyn Care for expert consultation and advanced spider vein treatment.
While most treated spider veins remain closed permanently, recurrence in the same location occurs in approximately 30–60% of patients within 3–5 years. Genetics, hormonal changes, or unresolved underlying vein issues may contribute.
Yes. People with darker skin types have a 1% to 30% risk of developing post-sclerotherapy hyperpigmentation. Hemosiderin and melanocytic stimulation play a role. It is dose- and technique-dependent.
High-impact exercises (running, jumping, heavy resistance, squats) are best avoided for at least 1–2 weeks, as they may increase vein irritation or bruising. Light walking is recommended immediately.
Moderate low-impact activities (e.g., brisk walking, cycling on flat terrain) can typically resume within 2–3 days after treatment. Strenuous exertion or endurance events should be postponed until after 1 to 2 weeks of healing.
Treating reflux or venous insufficiency before addressing spider veins helps reduce pressure in superficial vessels and decreases the chances of recurrence.
Most cases of hyperpigmentation resolve within weeks to a few months. However, in rare cases, it can take up to a year. Persistent discoloration beyond 12 months affects about 1–2% of patients.
Patients should avoid anti-inflammatory drugs like aspirin or ibuprofen for several days prior to treatment to minimize bleeding risk. Adequate hydration and avoidance of lotions on the day of the procedure are also advised.
Yes. When administered by trained specialists, combination approaches such as surface laser with sclerotherapy can be safely performed in a single session. However, precise planning is necessary to prevent adverse effects.
Engaging in regular physical activity, maintaining a healthy weight, avoiding prolonged sitting or standing, following a fiber- and antioxidant-rich diet, and refraining from tobacco use may reduce the risk of new vein formation.
Safe and effective treatment should be provided vascular specialists with training in sclerotherapy, laser systems, and imaging techniques such as transillumination or ultrasound. Proper sclerosant selection and application technique are also essential.
 Medically Reviewed By:
Medically Reviewed By: